Sorry for the slight delay releasing our “October” podcast – but here it is (note how it is cunningly labelled Episode 2)! This month we are reviewing the evidence for the pelvic binder and discussing scenarios in which it should (and should not) be used.
As always, please get in touch with questions and comments, either via the blog, twitter or email phemcast@gmail.com
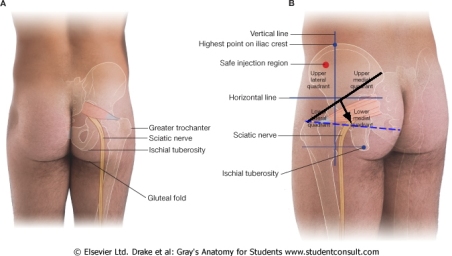
This is where the greater trochanters are:
This is where a binder should sit on the pelvis – it commonly ends up higher, either in application or ‘rides up’ during transfer – keep an eye on it!
These are the different types of fracture pattern that can occur in a pelvic fracture: of course patients can suffer from multiple force vectors so may end up with any combination of these fracture types.
Please click on this link below for our video on using a scoop to insert the pelvic binder…
As always… Get in touch!
References
- Scott I, Porter K, Laird C, Greaves I, Bloch M. The prehospital management of pelvic fractures: initial consensus statement. EMJ. 2013; 30(12): 1070-1072.
- Lee C, Porter K. The prehospital management of pelvic fractures. EMJ. 2007; 24: 130-133.
- Prasarn ML, Conrad B, Small J, Horodyski M, Rechtine GR. Comparison of circumferential pelvic sheeting versus the T-POD on unstable pelvic injuries: A cadaveric study of stability. Injury. 2013; 44: 1756-1759.
- Trebilcock H. Reducing overtriage and undertriage rates if pelvic fractures and unnecessary pelvic binder applications in major trauma patients. EMJ. 2015; 32(6): e17.
- DeAngelis NA, Wixted JJ, Drew J, Eskander MS, Eskander JP, French BG. Use of the trauma pelvic orthotic device (T-POD) for provisional stabilisation of anterior-posterior compression type pelvic fractures: A cadaveric study. Injury. 2008; 39: 903-906.
- Bottlang M, Krieg JC, Mohr M, Simpson TS, Madey SM. Emergent management of pelvic ring fractures with use of circumferential compression. The Journal of Bone & Joint Surgery. 2002; 84A (2): 43-47.
- Tan ECTH, van Stigt SFL, van Vugt AB. Effect of a new pelvic stabilizer (T-POD) on reduction of pelvic volume and haemodynamic stability in unstable pelvic fractures. Injury. 2010; 41(12): 1239-1243.
- Knops SP, Van Lieshout EMM, Spanjersberg WR, Patka P, Schipper IB. Randomised clinical trial comparing pressure characteristics of pelvic circumferential compression devices in healthy volunteers. Injury. 2011; 42(10): 1020-1026.
- Mason LW, Boyce DE, Pallister I. Catastrophic myonecrosis following circumferential pelvic binding after massive crush injury: A case report. Injury Extra. 2009: 84-86.
- Stewart M. BestBet: Pelvic circumferential compression devices for haemorrhage control: panacea or myth. EMJ. 2013; 30: 425-426.
- Croce MA, Magnotti LJ, Savage SA, Wood GW, Fabian TC. Emergent pelvic fixation in patients with exsanguinating pelvic fractures. Journal of American College of Surgeons. 2007; 204: 935-942.
- Knops SP, Schep NWL, Spoor CW, van Riel MPJM, Spanjersberg WR, Kleinrensink GJ, van Lieshout EMM, Patka P, Schipper IB. Comparison of three different pelvic circumferential compression devices: A biomechanical cadaver study. Journal of Bone & Joint Surgery. 2011; 93: 230-240.
- Knops SP, van Riel MPJM, Goossens RHM, Lieshout EMM, Patka P, Schipper IB. Measurements of the exerted pressure by pelvic circumferential compression devices. The Open Orthopaedics Journal. 2010; 4: 101-106.
How to cite this podcast:
Nutbeam T, Bosanko C. The Pelvic Binder. PHEMCAST. 2015 [cite Date Accessed]. Available from: http://www.phemcast.co.uk


Pingback: Episode 2: The Pelvic Binder | Prehospital and Retrieval Medicine - THE PHARM dedicated to the memory of Dr John Hinds
Really enjoying these podcasts, really useful as a new emergency medical technician. My only feedback would be the volume is a little low.
LikeLike
Thanks Simon, we’re working on it and hope sound quality will be better next time.
Clare
LikeLike
Oops, I left my comments for this podcast in the comment for podcast 1! Apologies, age related I’m sure 🙂
LikeLike
Loved both podcasts! Thank you, can I ask for a bit more advice on femur splintage with pelvic binders, I thought the kenrick was safe?
LikeLike
Hi Ashleigh
Thank you for the feedback!
The situation of combined suspected femoral and pelvic fractures is a difficult one – and I am afraid there are not many answers out there. Any device which works by traction against the pelvis (as they all seem to) will cause potential disruption / distraction of a pelvic fracture (particularly a vertical shear (VS) type pattern – typically caused by a fall from height).
The idea of the Kendrick Traction Device (KTD) as being perhaps a little better than others on the market was muted in the initial FPHEC consensus statement on the management of pelvic fractures – and seems to have become a urban legend. I discussed this directly with the manufacturers 3 years ago – they were very clear that the KTD was contraindicated in the presence of a pelvic fracture.
I have found that in the presence of a distal femoral fracture and suspected VS pelvic fracture the KTD can be attached distal to the pubic symphsis – relying on traction against skin and muscle to achieve alignment of the femoral fracture. I have also seen demonstrated the KTD used with axillary traction – though have always found this fiddly and impractical in my own practice.
We have a research project planned to further inform practice in this area – we will let you know how we get on!
I hope this is useful.
Kind regards
Tim
LikeLike
Wow- and yes extremely useful thank you! The auxiliary traction sounds fiddly. For now a ‘Mark 1’ hand straightening the leg will have to suffice.
Thank you so much!
Ash
LikeLike
Thanks guys for an awesomely good podcast.
I’m really interested in the comments about KTD use in the presence of a suspected pelvic # – have to admit that up until now I’d thought one of the real strengths of the KTD was exactly for the reason that it could be used when a pelvic # was present! Will now need to reconsider what I’ve been taught previously and what I teach to others!!
Cheers, Ed
LikeLike
Hi great podcast thank you. Looking forward to the video showing binder application using the scoop. We use Tpod and I find the application at scenes, whilst minimising movement, is often tricky.
LikeLike
Hi Tim, do you have a link please for the video showing applying pelvic binder using scoop ?
LikeLike
Thanks for the reminder Richard, we haven’t filmed it yet!
LikeLike
Hi Clare, Tim,
I am quite interested to hear your thoughts on the new NICE trauma guidance regarding fractures, particularly the clear guidance to wait until the patient is haemodynamicaly unstable for pelvic binder application.
The NICE guidelines are not as clear as the FPHC flowchart in the consensus statement.
If you are in a situation where you are at the patients side in quick time after injury, with a clear MOI, should we really be waiting until they have started to become compromised?
Thanks, looking forward to the next one.
LikeLike
Hi, thanks for the question. in the major trauma assessment guideline it says, ‘1.5.3 If active bleeding is suspected from a pelvic fracture after blunt high energy trauma: apply a purpose-made pelvic binder or consider an improvised pelvic binder, but only if purpose-made binder does not fit’, and the same text is included in the management of complex fractures guideline too. I can’t find the recommendation that you mention regarding haemodynamic instability but it seems to me that would be like shutting the stable door once the horse has bolted! I will continue to use the FPHC guideline: mechanism + clinical findings to guide binder application.
LikeLike
Pingback: emDOCs.net – Emergency Medicine EducationEM@3AM: Pelvic Ring Fracture - emDOCs.net - Emergency Medicine Education